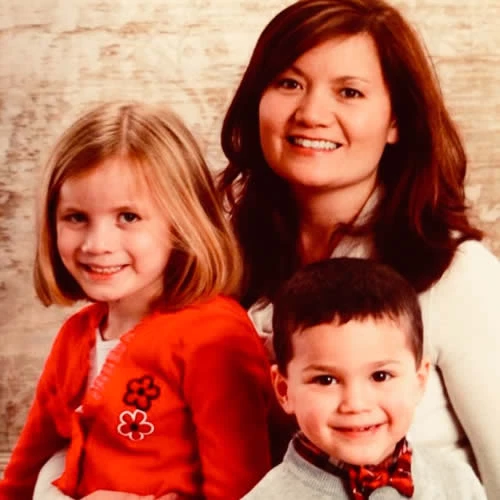
Clare Diagnosed at age 32
"It's the million dollar question we ask ourselves - when exactly did this uninvited cancer begin its intrusion?"
While I’ll likely never know the answer I begin my story a few years before my actual diagnosis. In 2011 during my first pregnancy, the nipple in my right breast became inverted. After my son was born, I had difficulty breastfeeding but was told I’m young and it’s quite normal for your breast to change during pregnancy. So for the next 2.5+ years, I went about my normal life, paying little attention to my breast. I eventually gave birth to my second child in November of 2013.
Once again I struggled to breastfeed but continued to convince myself there was no cause for concern. Then the summer of 2014 rolled around and I noticed not only was my nipple still inverted but my breast now seemed smaller. However, I felt no lump or tenderness and during my annual OB/GYN appointments I was lead to believe because I was young I needn’t worry. BUT by fall, my breast was not only misshapen it also ached. I knew I could no longer ignore these signs.
Finally in January, I made an appointment with my gynecologist to discuss my breast. After a quick exam, the doctor sternly instructed me to make an appointment with the breast surgeon ASAP. On January 28, 2015, eight days after my 32nd birthday, I walked into the breast surgeon’s office. I was originally scheduled to only have an ultrasound, but I soon found myself in the waiting room for a mammogram. As I looked around I noticed I was the youngest person by a decade or two (something I’d come to notice in most of the doctors’ offices I’d be frequenting throughout the upcoming year). After my ultrasound and mammogram the doctor called me back, swiftly took me into an empty room and said she had located a dense mass approximately the size of an orange behind my right nipple.
She quickly asked if my babies were taken care of because she wanted me to come back in 45 minutes during her lunch break to perform a biopsy. As I stood up she pulled me towards her and gave me a big hug and said “Us moms have to stick together, I’ve gotcha!” (Yes, my breast surgeon is an amazing human being).
After that appointment, I knew in my gut it was cancer. I received the official call about 36 hours later. I was informed I had Invasive Ductal Carcinoma; ER and PR positive Her 2 negative. Because my tumor was fairly large and sucking my breast in it was decided a mastectomy was necessary. Less than one week later I had my right breast removed as well as 7 lymph nodes with only macrometastatic disease in one node and micrometastatic disease in another. I was officially diagnosed with Stage IIb breast cancer and told I would need 4 rounds of chemo (cocktail combo - Taxotere and Cytoxan) every 3 weeks. I would also need to take a daily medication to address the hormonal aspect of my cancer (more on this in a minute). Radiation was undetermined at this time, which is why we did not do immediate reconstruction on the right breast. Chemo began in March. I did fairly well throughout my treatment.
As a stay at home mom, I found myself tired and worn down a lot faster chasing after my 3 and 1 year olds. I learned quickly how important it was to be diligent with my mouthwash regime – those mouth soars are nasty buggers. And because of my compromised immune system (and the fact that I lived with a preschooler and baby) I caught a couple of viruses and had two nasty cases of thrush. But I was lucky. I had an incredible support system of friends and family. They provided meals, childcare and more love than I could imagine. My husband was there every step of the way. We even spent our 5 year anniversary shaving my head…together.
As I wrapped up chemo, my breast surgeon suggested I make an appointment with the radiologist just to make sure radiation wasn’t necessary. Well, guess what? The radiologist ended up recommending radiation. During our initial meeting, he went back and forth but finally said he felt radiation was necessary because of my age (there is that age thing again). I was prescribed 30 rounds of radiation 5 days a week for the next 6 weeks. Again I was lucky to have had a subjectively routine experience with radiation (FYI - Aquaphor is a marvelous thing).
By August 2015, chemo and radiation were over. Don’t get me wrong it was amazing to know I’d grow hair again and wouldn’t have to put maxi pads around my raw radiated skin anymore but the hardest part (for me at least) was still to come – combating the hormonal aspect of my cancer. For this I was told I would need to take a daily pill (Anastrozole) to block my estrogen for the next 10 years (holy long time!), along with a Lupron shot every 12 weeks to suppress my ovaries. Sure a tiny pill sounds simple enough, but this particular pill accompanied by the shot proved to be anything but simple. The laundry list of side effects was brutal. So for the first time throughout my treatment, I began to question the plan.
I had never doubted my doctor’s ability to rid my body of cancer (something I’m eternally grateful for). I did, however, find myself quite disillusioned by their (specifically my oncologists) lack of consideration for quality of life after cancer. I was a young woman who would be experiencing menopause (and all the side effects) about 20+ years too early, and yet I was made to feel this was a non-issue. I was especially dumbfounded by the lack of information and concern shared in addressing any fertility issues. In searching for more information, I was able to make an appointment with Dr. Halle Moore of the Cleveland Clinic in November. And for the first time, I felt like the doctor was listening to my concerns not just as a cancer patient but as a real live – living – person. Dr. Moore explained (in a language I could understand) the importance of my hormonal treatment. She also helped me work through each of the side effects I was experiencing. She even addressed my desire to have more children.
She mentioned new studies addressing the possibility of taking a break during hormonal treatment to get pregnant and said it’s something we could discuss again further after completing a few more years of my hormone therapy. While there was no miracle answer during this visit, I did feel as though I had a better understanding of my treatment plan and was given the tools to deal with issues. And here I am now almost 15 months post diagnosis - cancer free. I am a few weeks away from wrapping up my reconstruction surgeries – woohoo! While my hormone therapy side effects have not disappeared I have found ways to better deal with them.
Throughout this journey, I’ve learned it’s ok to question the process. While there are countless resources out there for people affected by breast cancer, I still believe there are not enough for the growing younger population. I am grateful for local organizations like Pink Ribbon Girls whose services directly impact young breast cancer patients/survivors. And I look forward to becoming more involved in YSCs amazing efforts.
Are you a survivor, spouse, friend, or caretaker with a story to tell? We'd love to hear from you.